Tubal ligation
| |
|
Tubal ligation, also called getting one's tubes tied, is a form of sterilization. It works by stopping the egg cell from being able to travel through the fallopian tube to the uterus. For people who have a uterus, this procedure is meant to make it permanently virtually impossible for them to get pregnant. For some nonbinary people, if their only concern about their uterus is that a risk of pregnancy is a source of distress and body dissonance (called gender dysphoria), this is an alternative to removing the uterus (called hysterectomy). Tubal ligation has no effect on the person's menstrual flow, menstrual cycle, hormone balance, the ability to orgasm, cancer risk,[1][2] vulnerability to sexually transmitted infections,[3] or when or how the person will go through menopause.[4] Sometimes a person can choose to have uterine ablation done at the same time as tubal ligation, which is supposed to stop menstrual flow. If someone chooses to get ablation, then they have to get a tubal ligation or some other kind of contraception too.[5][6]
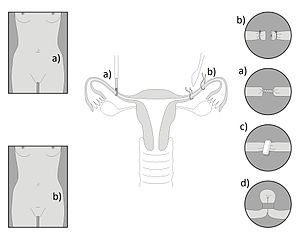
There are various methods for tubal ligation, which can be considered either a laparoscopic surgery (meaning it is done by cutting only a few tiny holes on the lower belly, and putting long thin laparoscope tools through them to do the work), or a procedure (meaning it can be done without cutting into the body). The fallopian tubes (which connect the ovary to the uterus) can be blocked off by a variety of different methods. The tubes can be tied and cut (ligation), clipped, pinched off in a loop with a band, burned (cauterization), blocked with scar tissue or an implant (tubal occlusion), or completely destroyed (salpingectomy). Any of these methods can be called tubal ligation on paperwork and health insurance. Cutting or tying the tubes has the most risk of still being able to get pregnant, whereas destroying the tubes is the most effective at preventing pregnancy. Blocking the tubes with an implant can be done by putting it in through the vagina, without cutting into the body, which is safer,[5] but an implant has the risk of later traveling into parts of the body where it is not supposed to be, which can be harmful.
Process
Some regions have laws that make it so that a person has to be certain age before they are allowed to get a tubal ligation. Tubal ligation is done by written informed consent from the patient, without needing a diagnosis of any health problem.
Anyone seeking sterilization will encounter sexist discrimination. Doctors, local laws, and health insurance companies put many more obstacles in the way of sterilization for people who they perceive as female, because of a widespread misconception that everyone who was born with a uterus will want to get pregnant someday. By comparison, doctors are much more willing and cooperative about giving the equivalent sterilization procedure to people who have testicles (a vasectomy). A doctor will only let a patient sign the consent forms for tubal ligation in the first place if the doctor is satisfied with how the patient answers a long series of intentionally offensive questions. Doctors intentionally try to lead people into giving the "wrong" answers, and then refuse to let the patient sign the consent forms. A survey found that male and female doctors are equally reluctant to let a "young" person (in their 20s or 30s) get a tubal ligation. Looking too youthful or whimsical can be enough for the doctor to decide you don't look like you can consider this decision, so dress maturely for this appointment.[7] See sterilization for more details on what the doctor wants to hear. There is also racist discrimination involved: doctors make sterilization relatively obtainable for people of color, or even push it on people of color who don't want it, but make sterilization almost impossible to obtain for people who are white. The motivation behind this racist discrimination is eugenics. After signing these consent forms, the patient may be required to wait a certain number of days before being allowed to have surgery, according to local laws or the person's health insurance. The wait is to give the patient time to make sure it's what they really want. This is also sexist discrimination, because people seeking a vasectomy are not forced to wait.[3][8][9] Even after submitting the consent forms, the doctors usually continue to create obstacles, such as deciding that the consent forms need to be redone because the doctor didn't print their name below their signature, or canceling the surgery at the last minute because the patient didn't call to confirm that they still wanted it.
A tubal ligation is done by a gynecologist, family medicine doctor, or general surgeon in a medical office, hospital, or clinic.[3] Tubal ligation is done in one stage. Although many sources refer to it being done under local or regional anesthesia,[10] typically it is done under general anesthesia. The patient goes home the same day.
During laparoscopic surgery, the surgeons put carbon dioxide gas into the abdominal cavity. This is to lift organs apart so that the surgeon can see what they're doing as they work. This is called insufflation of the abdomen. After surgery, the person's belly will still look distended. This is the only particularly uncomfortable part of tubal ligation. During recovery, the person may feel pain in their shoulders, because the distended abdomen puts pressure on the diaphragm, which the nerves refer to the shoulders.[11] The gas slowly goes away by being absorbed into the body, so in a few days, the belly will no longer look distended.
Costs and health insurance
A tubal ligation costs between USD$1,500 and USD$6,000.[3] Most health insurance companies cover it, especially if they otherwise cover contraception. If cost is a obstacle, you may be able to lower it to suit your income level through a state program or a Planned Parenthood health center.[3] If a complication happens, it could cost much more. See also: Saving up for transition expenses.
Complications and risks
Statistics show that sterilization by tubal ligation is safer than giving birth.[12] Since tubal ligation is a surgery done under general anesthesia, it has the same risks of any such surgery, plus a few of its own distinctive risks, depending on the method used. Like any surgery, the most common serious risks are from infection, complications from the anesthesia, and bleeding too much (hemorrhage).[12] Death from tubal ligation is extremely rare, and is usually caused by a reaction to anesthesia.[3]
During the surgery, there is a low risk that a bubble of air might get into a blood vessel (an embolism), which can cause the heart to stop (cardiac arrest). That can cause the patient to die on the operating table, but usually surgeons can restart the heart and resuscitate the patient.[13][14]
Sepsis is an extremely rare complication.
Tubal ligation does not increase the risk of cancer. In fact, tubal ligation correlates with a significantly lower rate of breast cancer[1] and ovarian cancer.[2]
Tubal ligation makes it virtually impossible to get a pregnancy of any kind. It is extremely rare for a pregnancy to happen afterward anyway, but it does happen. This can happen if the fallopian tubes weren't fully cut, tied, blocked, or destroyed, so that there was still enough of an opening in the tube for an egg or sperm to pass through. There is a tiny risk that if someone does get pregnant after a tubal ligation, then the embryo might implant in the wrong part of the uterus. This is called an ectopic pregnancy. Whether the embryo implants in the ovary (an ovarian pregnacy) or in the fallopian tube (a tubal pregnancy), it can cause the pregnant person to suffer circulatory collapse and die.[15] If someone gets an ectopic pregnancy, it is a life-threatening emergency that can only be fixed by removing the embryo (an abortion), which can sometimes only be done by surgery. For every 1,000 women who have their tubes cut, about 5 will later get pregnant, and of those, about 1 in 3 gets an ectopic pregnancy,[3] which is still much rarer than ectopic pregnancies in people who have not had a tubal ligation. For comparison, even if someone has had their uterus removed, but still has ovaries, there is still a chance that they could get an ectopic pregnancy. The only kind of surgery that makes it completely impossible to get pregnant is removal of the ovaries, but that means the person's body won't make hormones anymore.
See also
- Bottom surgery, meaning any of a variety of different surgeries that some nonbinary people may choose to get on their reproductive organs
- Practical resources
- Saving up for transition expenses
References
- ↑ 1.0 1.1 Brinton, L. “Tubal ligation and risk of breast cancer.” 2000.
- ↑ 2.0 2.1 Turney, Lyn. “Risk and contraception: What women are not told about tubal ligation.” Women’s Studies International Forum 16:5 (1993).
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 "Sterilization." Planned Parenthood. Retrieved July 9, 2020. https://www.plannedparenthood.org/learn/birth-control/sterilization
- ↑ Nelson, D. “Tubal ligation does not affect hormonal changes during menopausal transition.” 2005.
- ↑ 5.0 5.1 Donnadieu, A., et al. “Essure sterilization associated with endometrial ablation.” 2007.
- ↑ Donnadieu, A., and Fernandez. “The role of Essure stabilization performed simultaneously with endometrial ablation.” 2008.
- ↑ Misa, “How to get your tubes tied, even if you’re only 21.” http://misasplace.blogspot.com/2006/09/how-to-get-your-tubes-tied-even-if.html
- ↑ Erin Gloria Ryan, “Getting your tubes tied is a giant pain in the ass.” 2012-07-09. Jezebel. http://jezebel.com/5924414/getting-your-tubes-tied-is-a-giant-pain-in-the-ass
- ↑ J. Lowder, “Sterilize me, please.” Slate. http://www.slate.com/articles/double_x/doublex/2012/07/getting_your_tubes_tied_why_do_young_women_have_a_hard_time_getting_sterilized_.3.html
- ↑ Hatasaka, et al. “Laparoscopic tubal ligation in a minimally invasive surgical unit under local anesthesia compared to a conventional operating room approach under general anesthesia.” 1997.
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/003918.htm
- ↑ 12.0 12.1 Strauss, et al. “Sterilization-associated deaths: A global survey.” 1984.
- ↑ Duncan, C. “Carbon dioxide embolism during laparoscopy: A case report.” 1992.
- ↑ Ostman, P., et al. “Circulatory collapse during laparoscopy.” 1990.
- ↑ Raziel, et al. “Ovarian pregnancy—a 12-year experience of 19 cases in one institution.” 2003.